Inflammatory Bowel Disease
Ulcerative Colitis Overview

Ulcerative colitis is a disease in which the lining of the colon (the large intestine) becomes inflamed and develops sores (ulcers), leading to bleeding and diarrhea. The inflammation almost always affects the rectum and lower part of the colon, but it can affect the entire colon.
Although ulcerative colitis cannot be cured without removing the colon, it can usually be controlled. Most people with ulcerative colitis are able to live active lives. Controlling the disease usually means taking medications and seeing a gastroenterologist on a regular basis.
Ulcerative Colitis Causes
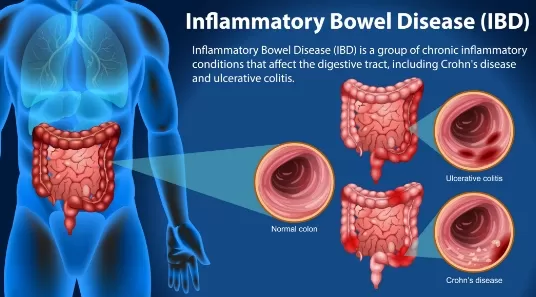
Ulcerative colitis is part of a group of conditions called “inflammatory bowel diseases” (IBD). Crohn’s disease is another inflammatory bowel disease, although that disease can affect the entire digestive tract (anywhere from the mouth to the anus), while ulcerative colitis only affects the colon.
Inflammatory bowel disease is not the same as irritable bowel syndrome (IBS).
Genetics and environmental factors both appear to play a role:
Ulcerative colitis tends to run in families, suggesting that genetics play a role. However, only about 10 to 25 percent of people with ulcerative colitis have a first-degree relative (either a sibling or parent) with inflammatory bowel disease (ie, either ulcerative colitis or Crohn’s disease).
When a person with a genetic susceptibility is exposed to a trigger (such as an infection, antibiotic, or something in the environment), the immune system can be activated. When this happens, the immune system recognizes the lining of the colon as foreign and attacks it, leading to inflammation.
In addition, ulcerative colitis can present after a person quits smoking. However, no single factor has been proven to be a known trigger in all situations.

Call us today for an appointment at Gledswood Hills or Shellharbour
Ulcerative Colitis Symptoms
The main symptom of ulcerative colitis is diarrhea, which may contain blood or mucus. People may also have abdominal pain and pain in the rectal area.
The symptoms of ulcerative colitis can be mild, moderate, or severe, and can fluctuate over time. Periods of active symptoms are called “flares.” When symptoms are under control and the colon is not inflamed, the ulcerative colitis is considered “in remission.”


Bowel symptoms
Ulcerative colitis is classified as mild, moderate, or severe based on symptoms.
People with mild disease may have:
- Mild diarrhea that may or may not be bloody (up to four
episodes per day) - Mild, crampy abdominal pain
- Straining with bowel movements
- Bouts of constipation
People with moderate disease may have:
- Frequent episodes of bloody diarrhea (more than four per
day) - Feeling tired or weak due to anemia (a low red blood cell
count) - Mild to moderate abdominal pain
- Low-grade fever


People with severe disease may have:
- Very frequent episodes of bloody diarrhea (six or more per
day) - Feeling tired or weak due to anemia (a low red blood cell
count) - Severe abdominal pain and cramping
- A racing heartbeat
- Fever
- Weight loss, which can happen quickly
Non-bowel symptoms
For reasons that are not well understood, people with ulcerative colitis can develop inflammation outside of the colon. Inflammation may affect large joints (hips and knees), causing swelling and pain. It can also affect the eyes, the skin, and the bile ducts (through which bile flows from the gallbladder and liver to the intestine, to help with digestion).
Some types of inflammation cause symptoms (for example, itchy eyes or red spots on the skin), while others are only detected when blood tests show an abnormality.
These symptoms usually occur during ulcerative colitis disease flares. However, inflammation can develop even when gastrointestinal symptoms are in remission.

Ulcerative Colitis Diagnosis

Ulcerative colitis may be suspected based upon your symptoms, physical examination, and laboratory test results.
To confirm the diagnosis, you will also need a procedure that allows your doctor to look inside your colon, such as sigmoidoscopy or colonoscopy. During these tests, the doctor takes small samples of tissue from inside your colon, which can be examined under a microscope in order to diagnose ulcerative colitis.
These tests also help rule out other conditions that can have similar symptoms, including Crohn’s disease, inflammation due to medications (such as non-steroidal anti-inflammatory drugs [NSAIDs] like Ibuprofen , or certain infections.
Ulcerative Colitis Management
The main goals of treatment for ulcerative colitis are to:
- Control symptoms (achieve remission)
- Prevent symptoms from coming back (maintain remission)
For most people, ulcerative colitis has a frustrating pattern of flares and remissions. However, about 15 percent of people who have an initial attack remain in long-term remission without medications, sometimes even for the rest of their lives.


Diet
Generally speaking, eating a well-balanced, nutritious diet can help you feel good and keep a healthy body weight. While there is no specific type of diet that has been proven to control inflammation in people with ulcerative colitis, some people do notice that certain foods seem to make symptoms worse.
For example, some people feel better if they avoid dairy foods like milk, yogurt, and cheese, while others may find that it helps to adhere to a low-fibre diet. If this is your experience, it is reasonable to avoid the foods that exacerbate your symptoms. If you do choose to modify your diet, it’s a good idea to talk with your health care provider to ensure that you are getting the nutrients your body needs and discuss whether you need to take supplements.
Avoiding medications that worsen symptoms
Pain relieving medications that contain nonsteroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen are not usually recommended if you have ulcerative colitis.
These medications can worsen symptoms. If you need to take a pain reliever, Paracetamol should not affect ulcerative colitis symptoms.


Treatment for mild to moderate symptoms
If your symptoms include rectal pain, rectal bleeding, and mild diarrhea, your treatment may include oral therapy as well as perhaps some topical medications that you apply directly into the rectum. The medication most often used first is called 5-ASA (aminosalicylic acid); it works by reducing inflammation in the rectum and colon.
If symptoms do not improve after several weeks, you might be recommended additional topical or oral glucocorticoid (steroid) medication and/or an oral 5-ASA medication.
Most people will experience symptom improvement soon after beginning treatment, and complete symptom relief after about four to six weeks. Continuous, lifelong treatment with a 5-ASA medication may be recommended to maintain remission.
Treatment of severe symptoms
If your symptoms are more severe (eg, six or more episodes of bloody diarrhea per day, often accompanied by additional symptoms), or a larger area of your colon is affected, you will be recommended a steroid medication, a biologic agent, or a small molecule:
Glucocorticoids cannot be used chronically, and they are tapered (ie, the dose is gradually reduced) once symptoms have improved. If severe symptoms continue, you may need treatment in the hospital with intravenous (IV) glucocorticoids or a different therapy for ulcerative colitis.
Biologic response modifiers or “biologics” are medications that have been used to treat Crohn’s disease and rheumatoid arthritis and are also used to treat ulcerative colitis. These include Adalimumab, adalimumab biosimilar. Infliximab, infliximab biosimilars Vedolizumab, Golimumab, or Ustekinumab. They work by interfering with pathways involved in inflammation, and they promote healing of the inflamed colon. These medications can be used to induce remission and, long-term, to maintain remission.
Biologics may be used alone or in combination with other treatments. Because of the potential risk of side effects, biologic agents are generally reserved for people with moderate to severe ulcerative colitis.
Small molecules are medicines that are taken by mouth and work on the immune system but act differently than biologics. Tofacitinib, Upadacitinib, and Ozanimod work within a few days to weeks to control moderately to severely active disease and can be used long term to control disease.
If symptoms do not improve
Some people do not respond, or respond only partially, to the treatments described above. These people are said to have “refractory” ulcerative colitis. This includes people who depend upon oral steroids to control their symptoms.
Treatments for refractory ulcerative colitis include:
Some patients may be admitted to the hospital for intravenous glucocorticoids (steroids). Most patients who respond have improvement in their symptoms usually within several days.
This is a powerful drug that was designed to prevent rejection after organ transplantation. It can be a very effective treatment to induce remission in people with refractory ulcerative colitis, although it cannot be used for life (ie, to maintain remission) due to potentially toxic side effects (risk of infection, kidney damage). This treatment is given in the hospital and once symptoms are under control, other treatments can be slowly substituted.

Call us today for an appointment at Gledswood Hills or Shellharbour
Ulcerative Colitis Surgery
People whose symptoms do not respond to medications, or who have difficulty with the side effects of their medications, sometimes choose to have their colon surgically removed.
There are several surgical procedures that may be recommended to treat ulcerative colitis. It is important to discuss all of the benefits and risks of surgery with your doctor, and also to have realistic expectations of the results.
The procedures can be divided into two groups:
- Those that require you to wear a bag to collect bowel
movements (permanent ileostomy) - Those that preserve your ability to control your bowel
movements (reattachment of anus/rectum)

During this procedure, the surgeon removes your colon, rectum, and anus; this is called proctocolectomy. The surgeon then attaches the ileum, or lower end of the small intestine, to an opening (ostomy) on the lower right side of the abdomen near the waistline. After this, your bowel movements will exit your body through the ostomy, rather than through your anus. You will wear a plastic bag on the outside of the ostomy to catch the bowel movements, and you will empty the bag as needed. While living with an ostomy can be challenging, especially at first, most people are able to live an active life once they get used to it. Your health care provider can help you learn how to manage your ostomy; it may also help to talk with other people who have had a similar experience.
One variation of this surgery involves creating a sac or pouch from the lower end of the small intestine that remains inside the lower abdomen to collect stool. Waste empties into this internal pouch. A small, leakproof opening is created in your abdomen so that you can insert a tube to drain the pouch.
This procedure is the most common surgery used to treat ulcerative colitis. During the procedure, the surgeon removes the large bowel and all or most of the rectum but preserves the anal sphincter or lower part of the rectum. The surgeon then creates a tubular pouch from the end of the small intestine and sews it to the anal canal or small part of remaining rectum.
This surgery allows you to continue to have bowel movements through your anus, and you will not need a permanent ileostomy. However, in most cases, you will require a temporary ileostomy while the new rectum heals. When the new rectum is healed, the temporary ileostomy is removed, and bowel movements will leave the body through the anal sphincter.
There is a risk of fecal leakage after this procedure, particularly at night. There is also a risk of recurrent ulcerative colitis in the end portion of the rectum.
Colorectal Cancer And Ulcerative Colitis

People with ulcerative colitis have an increased risk of colorectal cancer. Your risk of colorectal cancer is related to the length of time since you were diagnosed and how much of your colon is affected. In general, people who have had the disease for a longer time and those with larger areas of disease have a greater risk than those with a more recent diagnosis or smaller areas of disease involvement.
Colorectal cancer usually develops from precancerous changes in the colon, which grow slowly and can be detected with a screening test, such as colonoscopy.
In general, colonoscopy is recommended eight years after you first start having symptoms of ulcerative colitis. If this colonoscopy is normal, it is usually repeated every one to three years.