Gastroscopy
Gastroscopy or Endoscopy with Intervention

Overview
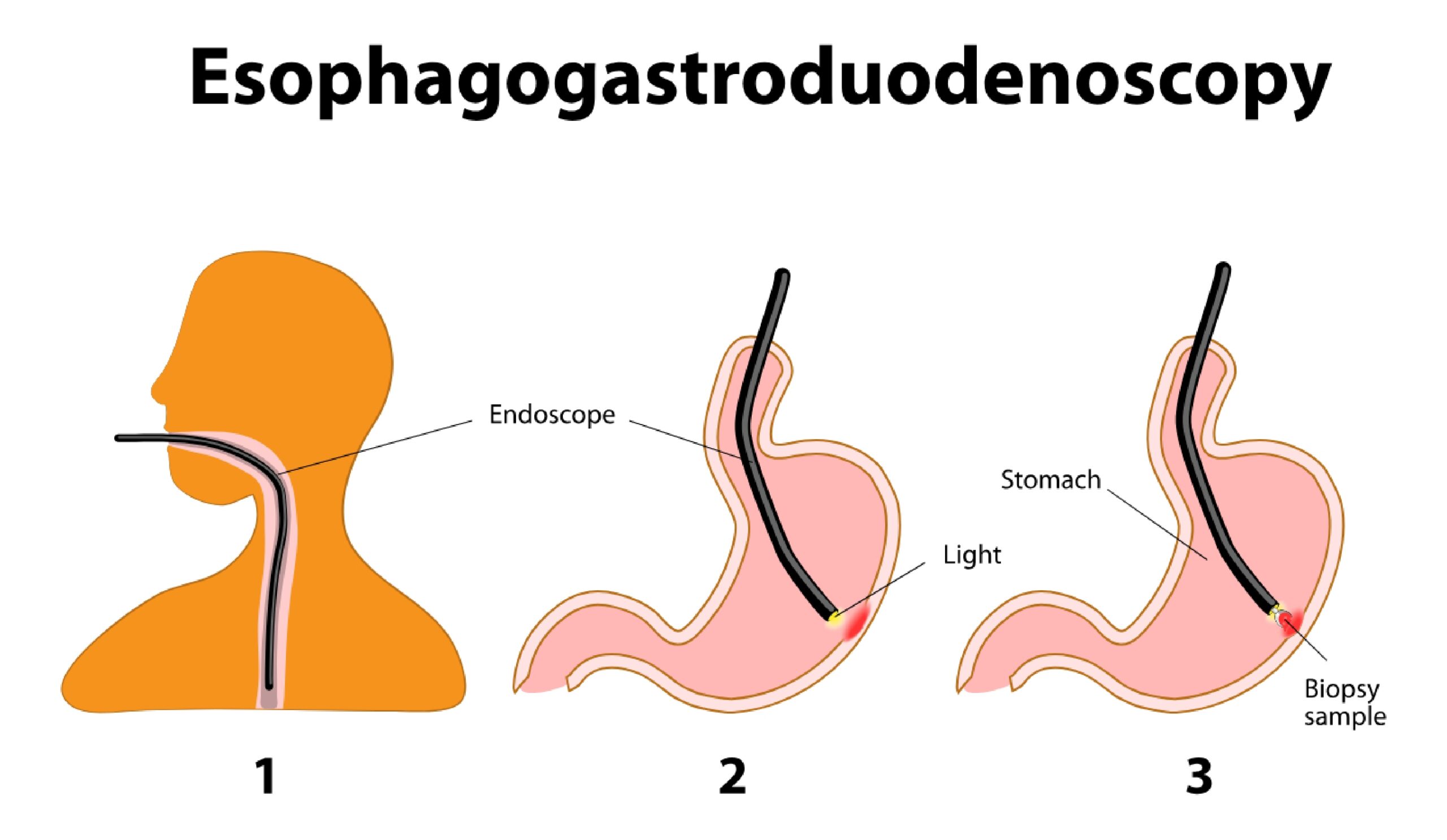
An upper endoscopy, often referred to as endoscopy, EGD, or esophago-gastro-duodenoscopy, is a procedure that allows a physician to directly examine the upper part of the gastrointestinal (GI) tract, which includes the esophagus, the stomach, and the duodenum (the first section of the small intestine.
The physician who performs the procedure, known as an endoscopist, has special training in using an endoscope to examine the upper GI system, looking for inflammation, bleeding, ulcers, or tumours.
Reasons for Upper Endoscopy
The most common reasons for upper endoscopy include:
- GERD or gastroesophageal reflux disease (often called heartburn).
- Unexplained discomfort or pain in the upper abdomen.
- Persistent nausea and vomiting.
- Upper gastrointestinal (GI) bleeding (vomiting blood or blood found in the stool that originated from the upper part of the GI tract). Bleeding can be treated during the endoscopy.
- Iron deficiency anemia (low blood count associated with a low iron level in the blood) in someone who has had no visible bleeding.
- Difficulty swallowing; food/liquids getting stuck in the esophagus during swallowing. This may be caused by a narrowing (stricture) or tumour or because the esophagus is not contracting properly. If there is a stricture, it can often be dilated with special balloons or dilation tubes during the endoscopy.
- Abnormal or unclear findings on an upper GI X-ray, CT scan, or MRI.
- Removal of a foreign body (a swallowed object).
- To check healing or progress on previously found polyps (growths), tumours, or ulcers.
Endoscopy Preparation
You will be given specific instructions regarding how to prepare for the examination before the procedure. These instructions are designed to maximize your safety during and after the examination and to minimize possible complications. It is important to read the instructions ahead of time and follow them carefully. Do not hesitate to call Dr Farah’s office or the endoscopy facility if there are questions.
You will be asked not to eat or drink anything for up to eight hours before the test. It is important for your stomach to be empty to allow the endoscopist to visualize the entire area and to decrease the possibility of food or fluid being vomited into the lungs while under sedation (called aspiration).
You may be asked to adjust the dose of your medications (such as insulin) or to stop specific medications (such as blood thinning medications) temporarily before the examination. Do not assume that you should either stop taking or continue taking any particular medication.
You should discuss your medications with Dr Farah before your appointment for the endoscopy and ask for instructions regarding what to do about your medications on the day before and the day of your procedure.
You should arrange for a friend or family member to escort you home after the examination. Although you will be awake by the time you are discharged, the medications used for sedation may cause temporary changes in the reflexes and judgment and interfere with your ability to drive or make decisions (similar to the effects of alcohol). Patients who receive sedation are generally required to be accompanied home after the procedure.


Call us today for an appointment at Gledswood Hills or Shellharbour
What To Expect
Prior to the endoscopy, the staff will review your medical and surgical history, including current medications and allergies. Dr Farah will explain the procedure and ask you to sign consent. Before signing consent, you should understand the benefits and risks of the procedure, alternatives to the procedure, and all of your questions should be answered.
If you are going to receive sedation for the procedure, an intravenous line (a needle inserted into a vein in the hand or arm) will be inserted to deliver medications. You may be given a combination of a sedative (to help you relax) and an opioid (to prevent discomfort), or other medications that are commonly used for sedation.
Your vital signs (blood pressure, heart rate, and blood oxygen level) will be monitored before, during, and after the examination.
The monitoring is not painful. Oxygen is often given during the procedure through a small tube that sits under the nose and is fitted around the ears. For safety reasons, dentures should be removed before the procedure. Often patients are asked not to wear or to remove jewellery and are discouraged from wearing nail polish to allow for easier monitoring of your oxygen level from your fingertip.
Although most patients are sedated for the examination, many tolerate the procedure well without any medication. Usually, these patients are given a medication to numb the back of their throats (either a gargle or a spray) just prior to the endoscopy to prevent gagging during the passage of the instrument. This may be offered to patients felt to be at higher risk for receiving sedation. Otherwise, if you are interested in having your endoscopy in this sedation-free manner, you should discuss this with the doctor beforehand to see if this is a possibility for you.
The Endoscopy Procedure

The procedure typically takes between 10 and 20 minutes to complete. The endoscopy is performed while you lie on your left side. A plastic mouth guard is placed between the teeth to prevent damage to the teeth and endoscope.
The endoscope (also called a gastroscope) is a flexible tube that is about the size of a finger. The endoscope has a lens and a light source that allows the endoscopist to see the inner lining of the upper gastrointestinal (GI) tract, usually on a TV monitor. Most people have no difficulty swallowing the flexible gastroscope as a result of the sedating medications.
Many people sleep during the test; others are very relaxed and generally not aware of the examination.
An alternative procedure called transnasal endoscopy may be available in some facilities. This involves passing a very thin scope (about the size of a drinking straw) through the nose. You are not sedated but a medication is applied to the nose to prevent discomfort. A full examination can be performed with this instrument.
The endoscopist may take tissue samples called biopsies. Obtaining biopsies is not painful. The endoscopist may also perform specific treatments (such as dilation [stretching of a narrowed area], removal of polyps, or treatment of bleeding), depending upon what is found during the examination. Air or carbon dioxide gas is gently introduced through the endoscope to open the esophagus, stomach, and intestine, allowing the endoscope to be passed through these areas and improving the endoscopist’s ability to see completely.
You may experience mild discomfort as air is pushed into the stomach and intestinal tract. This is not harmful; belching may relieve the sensation. The endoscope does not interfere with breathing. Taking slow, deep breaths just before and during the procedure may help you to relax.

Recovery from Endoscopy

After the endoscopy, you will be observed for a period of time, generally less than one hour, while the sedative medication wears off. Some of the medicines commonly used cause some people to temporarily feel tired or have difficulty concentrating. You typically will be instructed not to drive and not to return to work for the balance of the day of the procedure.
If you are breastfeeding, you may be advised to pump and discard the breast milk for the remainder of the day after receiving sedation medications.
The most common discomfort after the examination is a feeling of bloating as a result of the air introduced during the examination. This usually resolves quickly. Some patients also have a mild sore throat. Most patients are able to eat shortly after the examination.
Endoscopy Complications
Upper endoscopy is a safe procedure and complications are rare. The following is a list of some possible complications:
- Aspiration (inhaling) of food or fluids into the lungs, the risk of which can be minimized by not eating or drinking for the recommended period of time before the examination.
- Reactions to the sedative medications are possible; the endoscopy team (doctors and nurses) will ask about previous medication allergies or reactions and about health problems such as heart, lung, kidney, or liver disease, sleep apnea, and previous difficulties with sedation. Providing this information to the team ensures a safer examination.
- The medications may produce irritation in the vein at the site of the intravenous catheter. If redness, swelling, or discomfort occurs, you should call your endoscopist or primary care provider, or the number given to you at discharge. While this often can be treated by placing a warm compress on the area with pressure, sometimes the vein site can become infected and require further medical treatment.
- Bleeding can occur from biopsies or the removal of polyps, although if bleeding occurs, it is usually minimal and stops quickly on its own or can be easily controlled.
The endoscope can cause a tear or hole in the area being examined, also known as a perforation. This is a serious complication but fortunately occurs extremely rarely. If recognized immediately when it occurs, the endoscopist may be able to close the opening during the procedure. An open perforation is usually accompanied by considerable pain.
The following signs and symptoms should be reported immediately:
- Severe abdominal pain (more than gas cramps)
- A firm, distended abdomen
- Persistent Vomiting
- Any temperature elevation
- Difficulty swallowing or severe throat pain
- A crunching feeling under the skin of the neck
- Passage of red blood or black material in vomit or stool
After an Upper Endoscopy
Most patients tolerate endoscopy very well and feel fine afterwards. Some fatigue is common after the examination, and you should plan to take it easy and relax the rest of the day.
Dr Farah can describe the result of the examination before you leave the endoscopy facility. If biopsies have been taken or polyps removed, you should call for results at a time specified by the endoscopist, typically within one week.
