Inflammatory Bowel Disease
Crohn's Disease Overview

Crohn’s disease is a condition that affects the digestive tract. The cause of Crohn’s disease is unknown. The most common symptoms of Crohn’s disease include diarrhea, abdominal pain, weight loss, and fever. Some people with Crohn’s disease also have problems outside of the digestive tract, including a skin rash, joint pain, eye redness, and, less commonly, liver problems.
There is no cure for Crohn’s disease, but there are medicines that can help to keep the disease under control. If medicine does not control symptoms, surgery might be an option to remove the diseased part of the intestines.
Crohn’s disease is a condition that involves the body’s immune system, which normally fights infection but attacks healthy tissue instead. The cause of Crohn’s disease is not known. Having family members with Crohn’s disease increases the risk of developing the condition. When a person with an inherited risk is exposed to a trigger (an illness or something in the environment), the immune system is activated.
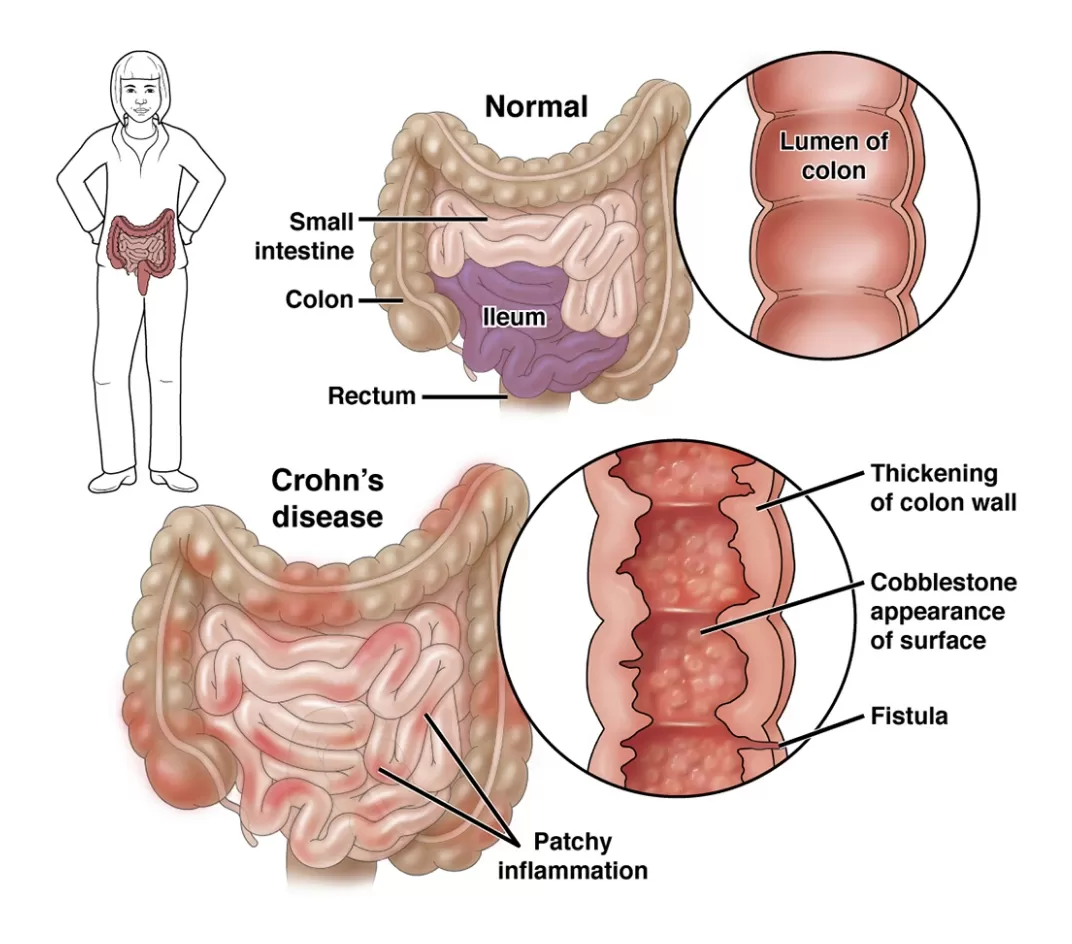
In Crohn’s disease, your immune system recognises the lining of your digestive tract as foreign and attacks it, causing inflammation. This inflammation causes the lining of your digestive tract to develop ulcers. Crohn’s disease usually affects the last part of the small intestine (called the “ileum”) and some of the large intestine (colon) but it can affect the entire digestive tract, from the mouth to the anus.
Crohn’s disease, like ulcerative colitis, is a type of inflammatory bowel disease. Inflammatory bowel disease should not be confused with irritable bowel syndrome.
There are several types of Crohn's disease:
This is when there is inflammation in the affected portion of the digestive tract.
This is when the inflammation causes scar tissue formation and narrowing of the bowel, leading to blockages.
This is when the inflammation burrows through all layers of the bowel and causes a track on the outside of the gastrointestinal tract to another part of the body. Most often fistulas occur from the bowel to around the anal canal, to another portion of the bowel, or to the abdominal wall.
Will I get better?
Crohn’s disease typically follows a repeating cycle of intermittent flares (when the condition worsens and symptoms are present) followed by periods of remission (when inflammation is controlled and symptoms are absent).
The pattern can be variable, with flares often lasting weeks to months and involving symptoms such as diarrhea and abdominal cramping.
Less commonly, there can be severe and disabling symptoms (such as severe abdominal pain and a blockage in the bowels). While 10 to 20 percent of people experience long-term disease remission after the initial flare, most people will continue to have disease flares. For anyone with Crohn’s disease, ongoing treatment increases the chance of entering and staying in remission.

Call us today for an appointment at Gledswood Hills or Shellharbour
Crohn's Disease Symptoms
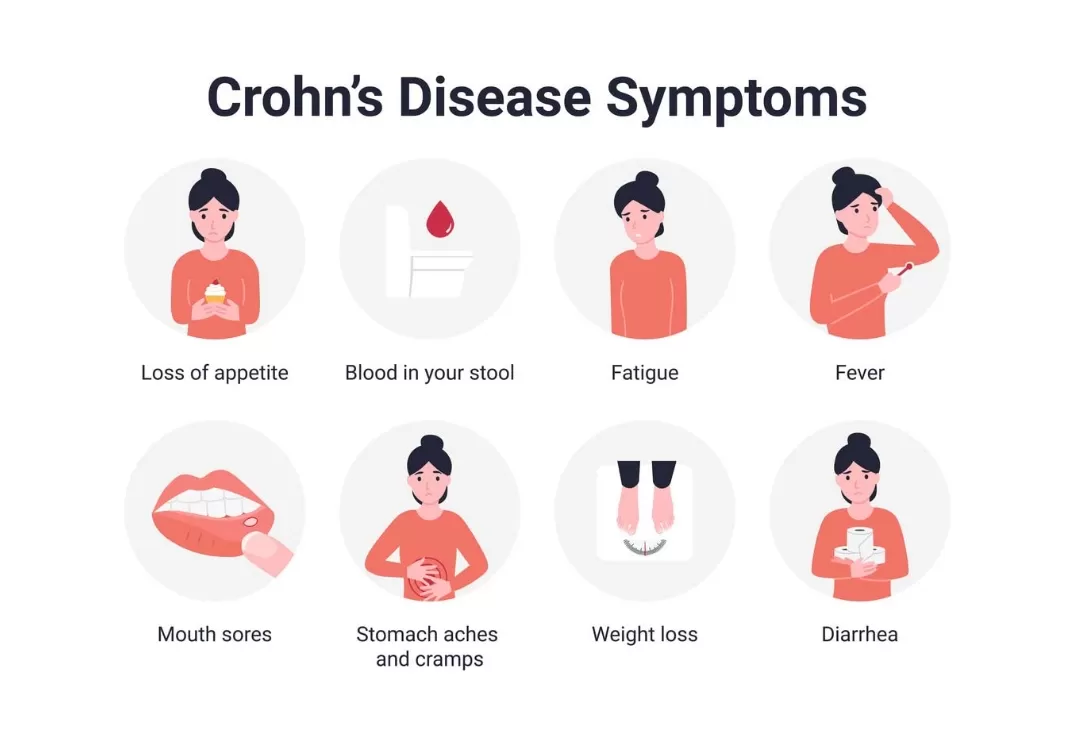
The most common symptoms of Crohn’s disease involve the digestive tract and include:
- Abdominal pain
- Diarrhea
- Fatigue
- Unintentional weight loss
- Anal/rectal pain
Some people get other symptoms and related disorders as well, including:
Mouth sores (called “aphthous stomatitis”) can develop during flares of Crohn’s disease. They are usually found between the gums and lower lip, or along the sides or underside of the tongue. Mouth sores are often painful. The medicines used to treat the digestive tract usually help to treat mouth sores as well.
Arthritis or joint inflammation can occur in people with Crohn’s disease. It usually affects the larger joints, and is most active when the bowel symptoms are active.
Inflammation of the eyes (called uveitis or scleritis) occurs in up to 5 percent of people with Crohn’s disease. These problems can affect one or both eyes. Symptoms of uveitis include “floaters” in the vision, eye pain, blurred vision, and sensitivity to light. Scleritis can cause burning or itching of the affected eye. Treatment usually includes eye drops.
Crohn’s disease can cause problems in the area around the anus. The most common problems include fissures (tears), ulcers, fistulas (a tunnel between the intestine and other organs), infected areas of skin, and stenosis (narrowing of the anus). These problems may occur alone or in combination.
Anal problems sometimes heal on their own without treatment. In other cases, treatment with medicines or surgery may be required. Soaking your bottom in warm water a few times a day and gently cleaning the area can help to speed healing.
Crohn's Disease Medications
There are a number of medications used to treat Crohn's disease. The "best" treatment approach will depend on several factors, including your age, which part of your intestine is affected, if your disease is severe, and the presence of other medical conditions you may have. The following is a summary of commonly used medications.
Steroids, or glucocorticoids, include Prednisolone and Budesonide medicines are usually used for a limited time to get inflammation under control and are then gradually stopped. Steroids are not recommended long-term because of the side effects. In addition, steroids do not heal the lining of the intestine like other therapies can.
The 5-aminosalicylates (abbreviated 5-ASA) are a group of medicines that reduce inflammation in the last part of the small intestine (ileum) and colon. 5-ASA medicines are used to treat ulcerative colitis (another type of inflammatory bowel disease), but in rare cases can be used for treating very mild and limited Crohn’s disease. For example, sulfasalazine can be used when the inflammation is found only in the colon.
Immunomodulators help to reduce the inflammation associated with Crohn’s disease. Immunomodulators might be recommended if you have severe symptoms or symptoms that do not improve with steroids, or if your symptoms worsen after decreasing your steroid dose. The most commonly used immunomodulators include Azathioprine, 6- Mercaptopurine and Methotrexate.
Biologic response modifiers (sometimes called “biologics”) are a class of therapies that work by preventing inflammation. These therapies can be used in combination with treatments described above.
Biologic response modifiers are expensive. They also have side effects that are different than other therapies because they are proteins rather than chemicals. As a result, biologic response modifiers are generally reserved for people with moderate to severe disease.
Biologic response modifiers are given either as an injection or through a vein (by IV); some can be given at home, while others must be given in a doctor’s office or infusion centre. Several biologic agents are available for treating Crohn’s disease, including:
In some cases, “biosimilar” medications are available. These are similar but not identical to biologic response modifiers, and they may be less expensive.
Biologic response modifiers interfere with the immune system’s ability to fight infection and should not be used in people with serious infections. You will need to get tested for tuberculosis (TB) before starting treatment with one of these medicines, since treatment can “activate” TB if you have been exposed to it previously (Biologic response modifiers can also reactivate hepatitis B, if present, and screening for this infection is important as well. Because these therapies are proteins rather than chemicals, some people have allergic reactions to them. Symptoms of an allergic reaction can include hives, rash, joint pain, or shortness of breath or wheezing.
Some studies have reported an association between biologics and a higher risk of developing lymphoma. More research is needed to determine how long a biologic response modifier can be used before the risk of lymphoma outweighs the benefits of the medication.
Small molecules are medications that are taken by mouth and work on the immune system but act differently than biologics.
In general, the use of antibiotics is reserved for treating complications of Crohn’s disease such as perianal fistula or abscess (an infected fluid collection).
Surgery For Crohn's Disease

Medicines can help control the symptoms and complications of Crohn’s disease and can help you to avoid or postpone surgery. However, surgery may be recommended if your symptoms are not controlled with medicine or if the side effects of medicine are unbearable. About 80 percent of people with Crohn’s disease will need surgery at some point in their life.
It is important to have realistic expectations of surgery. Surgery does not cure Crohn’s disease, but it can help you to feel better and return to normal activities. The disease eventually returns after surgery, and most people will need to keep taking medicines to control symptoms over the long term.
However, between 85 and 90 percent of people have no symptoms during the year following surgery. Up to 20 percent of people have no symptoms 15 years after surgery.
The most commonly performed surgeries for Crohn's disease include:
For this procedure, the surgeon removes the diseased part of the intestine (called a resection), then rejoins the two ends (called an anastomosis). After surgery, most people are still able to have bowel movements as usual, through the anus.
In some cases, the surgeon will not be able to reconnect the two ends of the intestine. Instead, the surgeon will connect the intestines to an opening in the abdomen through the skin, called an ostomy. Your bowel movements will exit your body through the ostomy, rather than through your anus. You will wear a plastic bag on the outside of the ostomy to collect the waste, and you will empty the bag as needed.
In most cases, the ostomy is temporary and is reversed after your bowel has healed for a few months. In other cases, a permanent ostomy is required.
The idea of an ostomy can be frightening. You will need to learn how to care for the ostomy, including how to care for the skin around the ostomy and fitting and emptying the bag that covers the ostomy. An ostomy nurse specialist is expert in the care of people with ostomies. With training, time, and support, it is possible to lead a normal life with an ostomy.
Strictureplasty is a procedure used to open blockages (strictures) in the bowel. It is sometimes done at the same time as a resection. Strictureplasty may be recommended if you have blockages in a particular part of your bowels over and over.

Call us today for an appointment at Gledswood Hills or Shellharbour
Crohn's Disease And Lifestyle
There might be certain foods or food groups that worsen your symptoms, particularly during flares, and it is reasonable to avoid these foods temporarily. However, eliminating entire food groups or severely restricting your diet can lead to undernutrition.
As an example, one study showed no difference in symptoms or disease activity for people consuming a very low carbohydrate (“low carb”) diet compared with a more balanced diet containing vegetables, fruits, and whole grains.
Your health care provider or a dietitian can help you make changes to your diet to help control symptoms.


Other lifestyle recommendations include the following:
- Regular exercise is a good idea for everyone, including people with Crohn’s disease.
- Smoking can worsen Crohn’s disease (ie, leads to more severe symptoms or more frequent flares) and increases your risk of needing surgery. While smoking has serious health risks for anyone, it is particularly important to avoid (or quit) smoking if you have Crohn’s disease.
- Avoid taking nonsteroidal anti-inflammatory drugs (NSAIDs) such as Ibuprofen since they can worsen the disease.
Crohn’s disease and colon cancer
Having Crohn’s disease increases your risk of developing colorectal cancer, but only in those who have Crohn’s disease affecting more than a third of their colon.
To find colorectal cancer as soon as possible, most experts recommend that people with Crohn’s disease start having colon cancer screening early and often. For some people, this might mean having a colonoscopy eight years after symptoms started, and then every one to two years thereafter.
Talk to your doctor to find out when you should start having colon cancer screening and how often it should be repeated.

Pregnancy And Crohn's Disease

If you have Crohn’s disease and want to get pregnant, Dr Farah can talk to you about what to expect.
More information about fertility, pregnancy, and breastfeeding in women with Crohn’s disease is also available separately.