Colon Polyps
Overview

The finding of polyps in the colon or rectum often raises questions for patients and their families. What is the significance of finding a polyp? Does this mean that I have, or will develop, colon or rectal (colorectal) cancer? Will a polyp require surgery?
Some types of polyps (called adenomas) have the potential to become cancerous, while others (hyperplastic or inflammatory polyps) have virtually no chance of becoming cancerous.
When considering risk from colon polyps, the following points should be considered:
- Polyps are common (they occur in 30 to 50 percent of
adults) - Not all polyps will become cancer
- It takes many years for a polyp to become cancerous
- Polyps can be completely and safely removed
The best course of action when a polyp is found depends upon the number, type, size, and location of the polyp. People who have an adenoma removed will require a follow-up examination as new polyps may develop over time and may need to be removed.

Colon Polyp Causes
Polyps are very common in males and females of all races who live in industrialised countries, suggesting that dietary and environmental factors play a role in their development.
Although the exact causes are not completely understood, lifestyle risk factors include the following:
- A high-fat diet
- A diet high in red meat
- A low-fiber diet
- Cigarette smoking
- Obesity
On the other hand, use of Aspirin and other nonsteroidal anti-inflammatory drugs and a high-calcium diet may have a protective effect.
Polyps and colorectal cancers are uncommon before the age of 40. Ninety percent of cases occur after the age of 50, with males somewhat more likely to develop polyps than females. Therefore, colon cancer screening is usually recommended starting at age 50 for both sexes. In certain situations and high risk patients, screening starts at an earlier age. It takes approximately 10 years for a small polyp to develop into cancer.
Polyps and colon cancer tend to run in families, suggesting that genetic factors are important in their development.
Any history of colon polyps or colon cancer in the family should be discussed with your doctor, particularly if cancer developed at an early age in the family member, in close biological relatives, or in multiple family members. As a general rule, screening for colon cancer begins at an earlier age in people with a family history of cancer or polyps.
Some rare genetic diseases increase the chances of getting colorectal cancer relatively early in adult life. Familial adenomatous polyposis and MUTYH-associated polyposis cause multiple colon polyps. Another hereditary nonpolyposis colon cancer, or Lynch syndrome, increases the risk of polyps and colon cancer. Testing for these genes may be recommended for families with high rates of cancer. People diagnosed with colorectal cancer should have genetic testing, which may identify the presence of some of these conditions.

Call us today for an appointment at Gledswood Hills or Shellharbour
Types of Colon Polyps
The most common types of polyps are hyperplastic and adenomatous polyps. Other types of polyps can also be found in the colon, although these are far less common and are not discussed here.
Hyperplastic polyps are usually small, located in the end-portion of the colon (the rectum and sigmoid colon), have no potential to become malignant, and are not worrisome. It is not always possible to distinguish a hyperplastic polyp from an adenomatous polyp based upon appearance during colonoscopy, which means that hyperplastic polyps are often removed or biopsied to allow microscopic examination.
Two-thirds of colon polyps are adenomas. Most of these polyps do not develop into cancer, although they have the potential to become cancerous. Adenomas are classified by their size, general appearance, and specific features as seen under the microscope.
As a general rule, the larger the adenoma, the more likely it is to eventually become a cancer. As a result, large polyps (larger than 5 millimeters) are usually removed completely to prevent cancer and for microscopic examination to guide follow-up testing.
Polyps that contain cancerous cells are known as malignant polyps. The optimal treatment for malignant polyps depends upon the extent of the cancer (when examined with a microscope) and other individual factors.
Colon Polyp Diagnosis

Polyps usually do not cause symptoms but may be detected during a colon cancer screening examination (such as flexible sigmoidoscopy or colonoscopy) or after a positive screening test for occult blood in the stool.
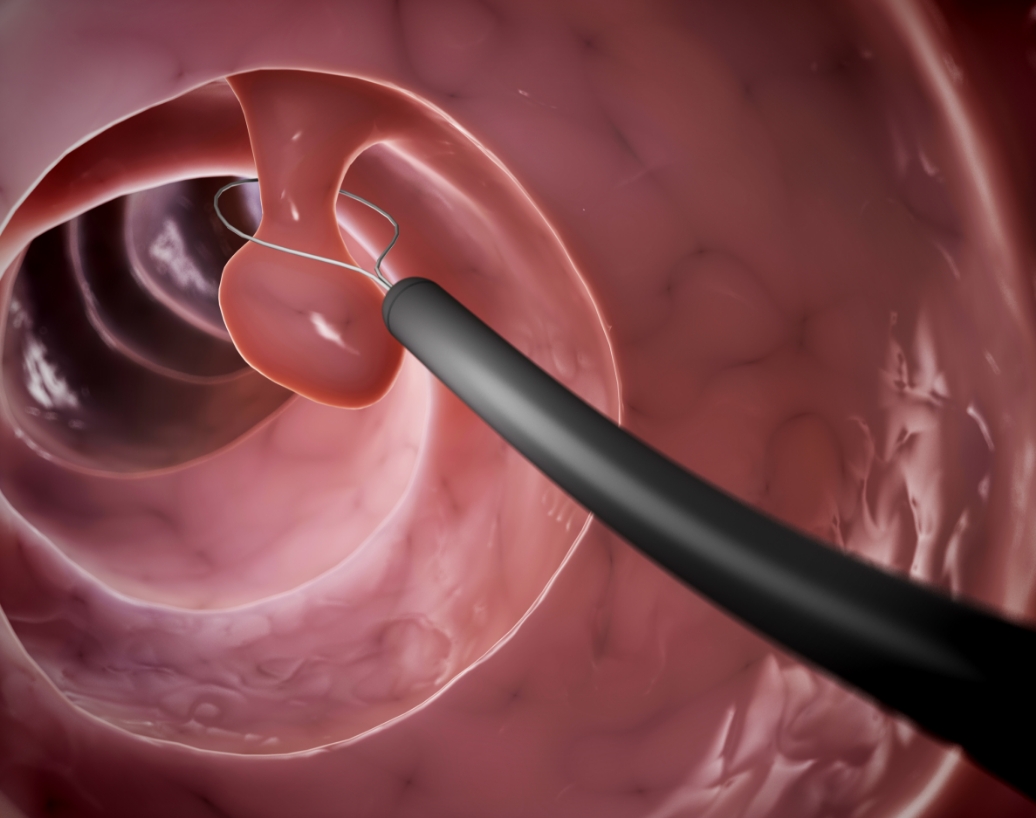
Colonoscopy is the best way to evaluate the colon for polyps because it allows the clinician to see the entire lining of the colon and remove most polyps that are found (occasionally, large polyps need to be removed during a separate procedure).
During colonoscopy, a clinician inserts a very thin, flexible tube with a light source and small camera into the back passage. The tube is advanced through the entire length of the large intestine (colon).
The inside of the colon is a tube-like structure with a flat surface with curved folds. A polyp appears as a lump that protrudes into the inside of the colon.
The tissue covering a polyp may look the same as normal colon tissue, or there may be tissue changes ranging from subtle color changes to ulceration and bleeding. Some polyps are flat (“sessile”) and others extend out on a stalk (“pedunculated”).
Colonoscopy is the best test for the follow-up examination of polyps. Virtual colonoscopy using computed tomography technology is another test used to detect polyps.

Colon Polyp Removal
Colorectal cancer is preventable if precancerous polyps (ie, adenomas) are detected and removed before they become malignant (cancerous). Over time, small polyps can change their structure and become cancerous. Polyps are usually removed when they are found on colonoscopy, which eliminates the chance for that polyp to become cancerous.
Procedure
The medical term for removing polyps is polypectomy. Most polypectomies can be performed through a colonoscope. Small polyps can be removed with an instrument that is inserted through the colonoscope and snips off small pieces of tissue.
Larger polyps are usually removed by placing a noose, or snare, around the polyp base and burning through it with electric cautery. The cautery also helps to stop bleeding after the polyp is removed.
Polyp removal is not painful because the lining of the colon does not have the ability to feel pain. In addition, a sedative medication is given before the colonoscopy to prevent pain caused by stretching of the colon. Rarely, a polyp will be too large to remove during colonoscopy, which means that a surgical procedure will be needed at a later time.
Types of Polypectomy
Cold and Hot snare Polypectomy
This is a specialised form of Polypectomy that allows the Gastroenterologist to remove large flat or sessile polyps during colonoscopy, whereas in the past these polyps would have required surgery. Using this technique, polyps of almost any size can be removed, so long as they have not yet turned cancerous. This can generally be determined through careful inspection of the polyp, or with biopsy.
The technique of EMR involves the injection of a specialised solution* into the bowel wall (submucosa) just below where the polyp is attached. This lifts the polyp up off the bowel wall on a cushion and means the polyp can be safely snared off either in one or many pieces, until it has been completely removed. Colonoscopy with EMR carries a slightly higher risk than normal procedures with around a 0.5% chance of bowel perforation and 5-10% chance of post procedure bleeding.
* The solution is made up of a volume expanding type of intravenous fluid (Gelofusine®, Voluvan®), mixed with blue dye to highlight the polyp tissue (methylene blue) and a tiny amount of adrenaline to prevent bleeding.
This is a variant of EMR in which a specialised needle knife is used to dissect lesions away from the submucosa, in one piece. This technique is typically not required for colon polyps because the majority of colon polyps are benign, so they can be removed piecemeal with a low recurrence risk.
Complications
Polypectomy is safe although it has a few potential risks and complications. The most common complications are bleeding and perforation (creating a hole in the colon). Fortunately, this occurs infrequently (one in 1000 patients having colonoscopy).
Bleeding can usually be controlled during colonoscopy by cauterizing (applying heat) or applying endoclips to the bleeding site; surgery is sometimes required for perforation.

Follow-up Colonoscopy
The results of the tissue analysis of polyps are discussed with patients when they are available, within a few weeks after the procedure, to decide if and when a follow-up examination is needed.
People with adenomatous polyps have an increased risk of developing more polyps. There is a 25 to 30 percent chance that adenomas will be present on a repeat colonoscopy done three years after the initial polypectomy.
Some of these polyps may have been present during the original examination but were too small to detect. Other new polyps may also have developed.
Repeat colonoscopy is usually recommended. The exact time interval for follow-up varies depending upon several factors:
- Microscopic characteristics of the polyp.
- Number and size of the polyps.
- Whether it was possible to examine the entire colon.
- Ability to see the colon during the colonoscopy. A bowel reparation is needed before colonoscopy to remove all traces of faeces (stool). If the bowel preparation was not adequate enough, faeces may remain in the colon, making it more difficult to see small- to moderate-size polyps. In such situations, when the colonoscopy was not adequate, it should be repeated to ensure adequate visualization.
Screening saves lives. Persons who undergo regular screening for colon cancer are much less likely to die from colon cancer. Following the screening guidelines can also prevent people from developing colon cancer.


Lifestyle measures
Guidelines issued by one of the major medical societies in the United States (the American College of Gastroenterology) suggest the following:
- Eat a diet that is low in fat and high in fruits, vegetables,
and fibre - Maintain a normal body weight
- Avoid smoking and excessive alcohol use
Implications for the Family
First-degree relatives (a parent, brother, sister, or child) of a person who has been diagnosed with an adenomatous polyp or colorectal cancer before the age of 60 years, or those with two or more relatives with colorectal cancer at any age, have an increased risk of developing adenomatous polyps and colorectal cancer compared with the general population.
Thus, a person diagnosed with an adenoma or colon cancer should share the information with family members, and each person should learn about the cancer history in their family. Some genetic conditions, such as Lynch syndrome, can also cause other cancers.
While screening for polyps and cancer is recommended for everyone (typically beginning at age 45), those at increased risk should begin screening earlier. The best test for screening in people with an increased risk of cancer is not known, although a sensitive test (such as colonoscopy) is usually recommended.

Relatives can be told the following, based on typical guidelines for screening people with a family history of colorectal cancer:
People who have one first-degree relative (biological parent, brother, sister, or child) with colorectal cancer or an advanced type of adenomatous polyp at a young age (before the age of 60 years), or two first-degree relatives diagnosed at any age, should begin screening for colon cancer earlier, typically at age 40, or 10 years younger than the earliest diagnosis in their family, whichever comes first. Screening usually involves colonoscopy, which should be repeated every five years.
People with a second-degree relative (grandparent, aunt, or uncle) or third-degree relative (great-grandparent or cousin) with colorectal cancer should be screened for colon cancer similar to a person with an average risk.
- Some conditions, such as hereditary nonpolyposis colorectal cancer (Lynch syndrome), familial adenomatous polyposis, MUTYH-associated polyposis, and inflammatory bowel disease (eg, ulcerative colitis, Crohn disease) significantly increase the risk of colon polyps or cancer in family members. Colon cancer screening in this group is discussed separately.